Stage one: Pathway mapping
The first stage of this project was an eight-month scoping period, during which the project lead, Fiona Munro, met with practitioners working across Scotland to gain an understanding of the pathways already in place, what was working well and what could be improved.
During this phase, practitioners were invited to participate in a pathway mapping activity to visually represent the pathways in their area. When discussing the pathway, practitioners tended to focus on the problems they faced when discharging an older person from acute care. This provided insight into many pathways and processes across Scotland and the challenges associated with ensuring a positive experience.
A number of practitioners, working across all three sectors, were involved in this process. This led to a number of varying perceptions of the problems within the pathway and the associated causes. This made synthesising the practitioners’ overviews difficult. As a result, the maps are not meant to represent what the ideal pathway should look like but rather they simply offer a high level view of what older people may experience when discharged from hospital in Scotland and the challenges associated with ensuring older people are discharged through a positive pathway.
During this phase a summative literature review of the key problems and solutions, and a list of key resources for further reading was also established.
An overview of this phase of the project, alongside thoughts and insights on the project from Peter Macleod (Director of Social Work at Renfrewshire Council and newly-appointed Chair of the Iriss Board), can be found in a special Hospital to Home episode of Iriss.fm.
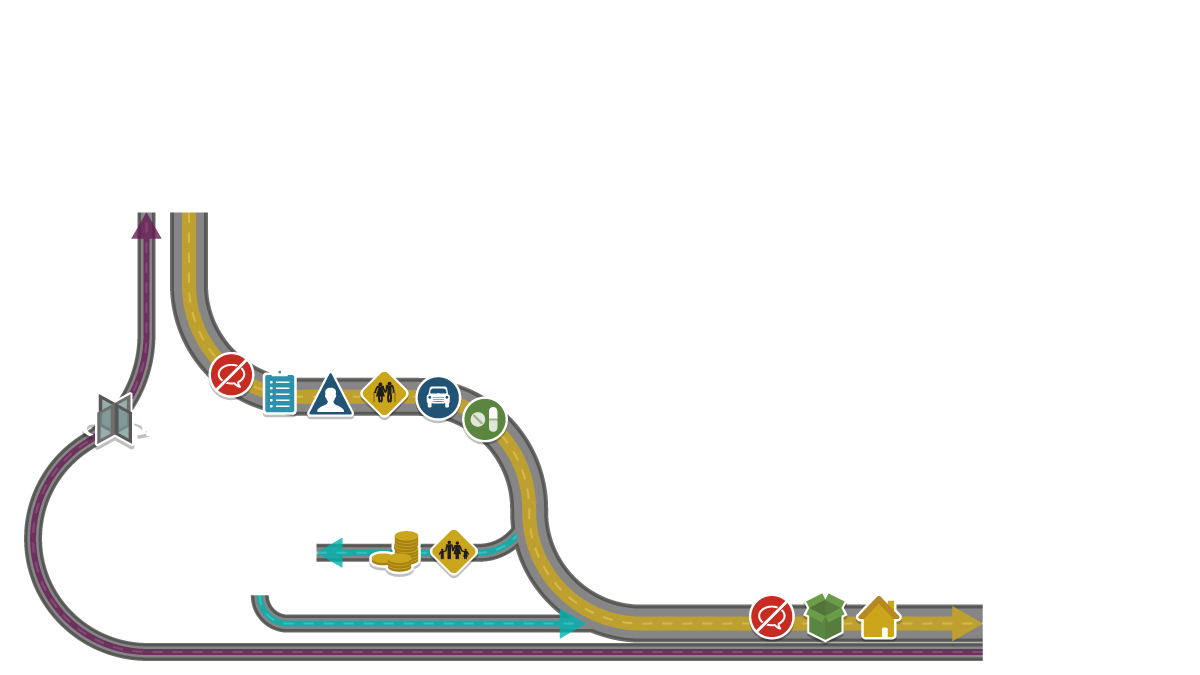
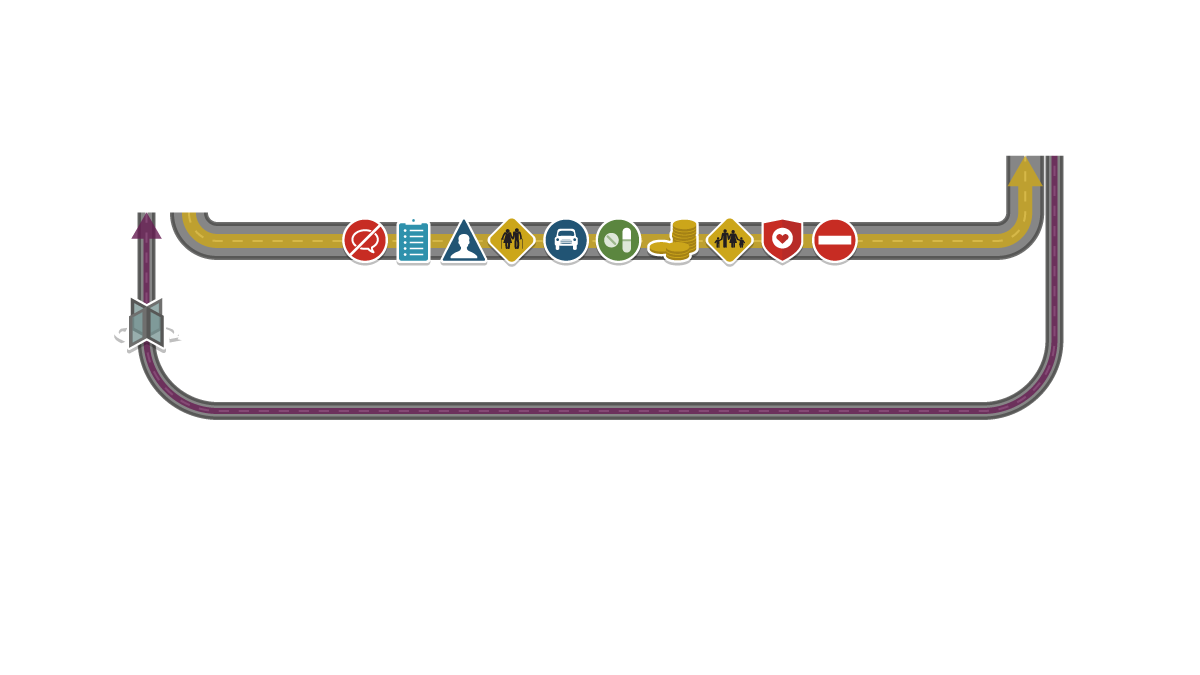
The pathway map
The information gathered during the first phase of the project identified the four most common pathways for older people when they leave hospital:
- Straight home (with or without family support)
- Early supported discharge or intermediate care at home
- Step down or intermediate care
- Straight to a care home
Using the pathway map
Please use the four numbered tabs to view each pathway. Click on the icons positioned within these pathways to gain an understanding of some of the problems and associated solutions discussed by practitioners across Scotland.
Pathway one: Straight home
The majority of older people can be discharged straight to their own home with support from unpaid carers and existing, new or increased care packages. Many older people are independent, or will recover quickly at home and do not require support to return home.
In some circumstances where an older person needs some support but not health or social care input, family or friends may offer a place to stay following discharge from hospital, before returning to their own home. This allows them to leave acute care and benefit from support from people they know.
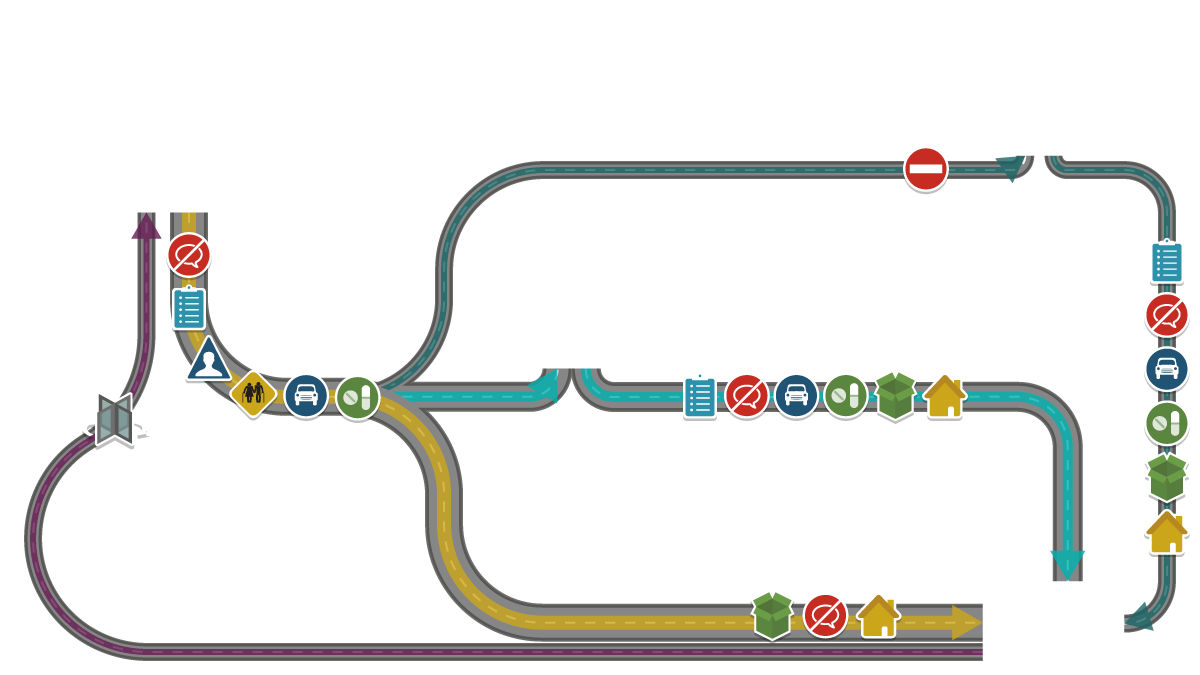
Pathway two: Early supported discharge or intermediate care at home
An older person may be discharged home from hospital with Early supported discharge (ESD) or Intermediate Care at Home in place. This is where the older person receives further treatment, rehabilitation and support in their own home for a period of two to six weeks depending on their care needs. A key aspect of this pathway is that the care and support can be increased or decreased depending on individual needs.
In some cases older people may need continued support via homecare, a district nurse or a community care package following ESD to ensure they are not readmitted to hospital.
Pathway three: Step down or intermediate care
Some older people who are no longer acutely unwell but have continuing rehabilitation needs that are unable to be met at home in the short term will transfer to a ‘Step Down’ or Intermediate Care bed in a care home or community hospital before returning home.
Step Down beds allow the person to be discharged from an acute setting that no longer meets their needs, helps to reduce the risk of healthcare associated infections (HAIs) and allows the older person to move closer to their own home and community.
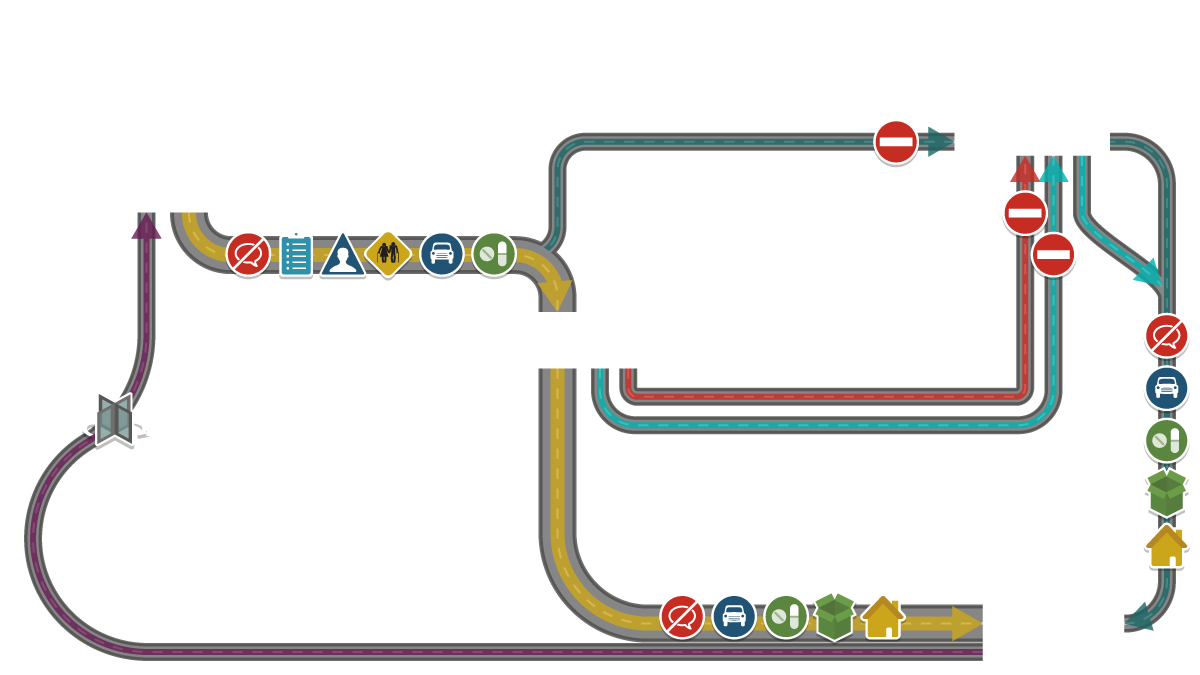
Pathway four: Straight to a care home
A minority (< 10%) of older people may be discharged from hospital straight to a care home. The exact figure is reported locally but not nationally. This may happen following a number of readmissions, over time, and where the multi-agency assessment is that care at home is no longer able to satisfy the individual's increasing needs.
It would be preferable if the older person's increased care requirements were identified whilst they were still at home so that they could be transferred to a care home directly from their own home without the need for unnecessary admission or delays in an acute care setting.

Literature
Problems identified in the literature
At point of admission
The majority of hospital admissions for older people are unplanned. More needs to be done to support older people at the point of admission to hospital and to prevent unnecessary admissions.
During discharge planning
During early discharge planning within acute settings there is often little engagement with the older person receiving care, their family or their informal carer about decisions concerning their discharge and ongoing care arrangements. As a result, older people and their families and/or informal carers are not routinely asked about their home circumstances, nor how they will cope following discharge.
Furthermore there is a lack of communication between acute care and outside agencies such as GPs, local authorities and community based care providers at this early stage in the planning. This can cause delays later in the pathway when these agencies are given insufficient time to accommodate a discharge.
At point of discharge
Transportation is a major issue when discharging an older person from hospital either to their home, a community hospital or a care home. Lack of communication between the acute setting and community based service providers means that there is often inadequate notice of discharge and transport is often requested with less than 24 hours notice, resulting in the older person being unnecessarily delayed in acute care.
Medication issues often arise due to lack of communication between health practitioners in acute and primary care settings. This can often result in an unnecessary readmission to acute care.
Following discharge, older people often experience delays or inadequacies in the provision of community based services, resulting in little assistance if the appropriate care packages are not in place at the time of discharge. As older people often live alone, this can mean they go unsupported for some time, again, resulting in an unnecessary readmission.
Essential aids such as commodes are usually provided before or 'soon after' discharge but it can be several weeks or even months for other aids or adaptations to be put in place.
Solutions identified in the literature
Strategic
There needs to be closer communication throughout all aspects of the pathway: between acute and community health, health and social care, housing and wider community organisations. The implementation of the integration agenda offers a renewed opportunity to transcend these traditional boundaries. It will, however, require that the delivery of good quality outcomes for the individual is a priority.
There is a need for central government action in order to overcome the financial, legal and administrative obstacles to joint working. This will support health care, social care and housing agencies to work in partnership with one another to increase their own internal efficiency and develop shared solutions to local problems.
There needs to be improved links and communication resource links between health professionals based in acute and primary care at all stages in the pathway to ensure problems arising from medication changes are overcome and readmissions are reduced.
Prior to admission
Wherever possible the discharge should be planned before or at the point of admission. This would be supported by identification of all problems likely to arise being identified early alongside the appropriate action that would be taken in this event. Older people should undergo early screening prior to or at the point of admission to allow this information to be fed into their discharge plan. As part of this, multidisciplinary teams should be allocated clear lines of responsibility. In cases of unplanned admissions, they should also experience an early review by a senior clinician in the emergency department at point of admission.
During discharge planning
There is a need for acute care to take a collaborative and multidisciplinary approach to discharge planning at an early stage in the older person's pathway either prior to or at the point of admission. This would be supported by ongoing and effective communication throughout the planning process between the older person, their family, health and social care professionals within acute and primary care and community services. In addition, improved relationships and effective communication channels are essential between health and social care practitioners working in the acute setting and those based in the community.
It may also be advantageous to employ a designated (named) person to ensure that all stages of the discharge plan are fulfilled and to ensure that the discharge is timely and linked to appropriate support services within the community.
A 'discharge checklist' could be put in place to address: primary care workloads; social work assessment; ambulance transport; discharge prescription; social services; day hospital; continuing care facilities; housing. This information could then be shared with all those involved in the pathway including hospital and community based practitioners, the older person, their family and informal carer.
At point of discharge
Progress has been made towards the pathway from hospital to home and discharge process becoming outcomes-focused and person-centred but more still needs to be done. This will require ongoing monitoring to ensure the older person's outcomes are being met.
Further reading
Please visit our Learning Exchange collection for a list of suggested further reading.
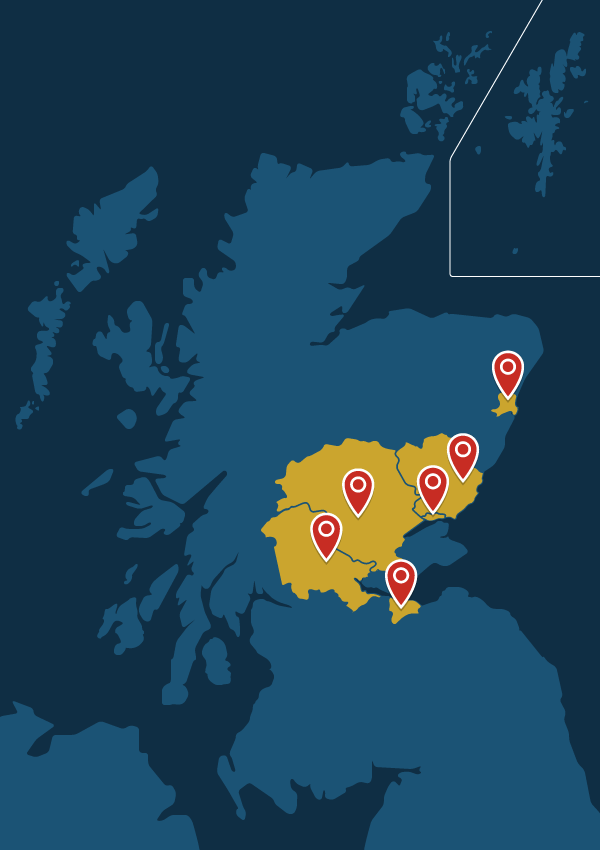
Localities
This localities map is based on practitioners' experiences and provides a 'snap shot' of what was happening in Scotland during the initial eight-month scoping phase of the project. If you'd like to contribute the view from your area we'd love to hear from you.
Using the localities map
Please click on the localities, either within the map or below, to gain an overview of the pathway from hospital to home in each area. Within these localities you'll find written case studies and also some audio descriptions from practitioners working within that area.
The featured localities are:
The people
Many people were involved throughout the initial scoping phase of the project, supporting insight into the pathways older people may experience in Scotland during their transition from hospital to home.
With special thanks for their time and input, and with their permission, some of those involved are listed below:
National Project Advisory Group
- Bernie Campbell: Scottish Care
- David Strathearn: CCPS Associate / Voluntary Sector Advisor
- Diane McCulloch: Head of Community Care, Social Work Department, at Dundee City Council
- Miles Witham: Clinical Reader in Ageing and Health at NHS Tayside/University of Dundee School of Medicine
- Roy Soiza: Consultant Geriatrician & Honorary Clinical Senior Lecture at NHS Grampian
National Support
- Anne Kidd: Chief Executive Officer, Voluntary Action East Renfrewshire
- Amanda Clements: Nurse Coordinator Intermediate Care P&K CHP
- Caroline McQuillian: Associate Nurse Director NHS Tayside, Nursing & Midwifery Directorate
- Cesar Rodriguez: Clinical Lead Older People in Acute Care Collaborative, NHS Tayside
- Deirdre Gallie: Delayed Discharge Coordinator, NHS Forth Valley
- Eleanor Cunningham: Acting Strategic Policy and Performance Manager, Department of Health and Social Care, City of Edinburgh Council
- Gordon Gray: Assistant Programme Manager – Delayed Discharges at NHS Lothian / JIT Action
- Helen Allbutt: Lead for Research Governance at NES – NHS Education for Scotland
- Jane Davidson: JIT Action Group
- Karen Anderson: Head of Allied Health Service at Dundee CHP, NHS Tayside
- Lynne Morman: Resource Manager, Social Work Department
- Lynne Wardle: Director, Taylor Haig
- Mary Taylor: Chief Executive at Scottish Federation of Housing Associations
- Mavis Leask: Care Manager (Angus Council)
- Prof Stewart Mercer: Chair in Primary Care Research (General Practice and Primary Care) at University of Glasgow
- Susan Gunn: Celebrate Age Network (CAN) Forum
- Susan Nevil: Organisational Development Consultant (Health and Social Care Integration) Perth and Kinross Council
- Tracey Passway: Clinical Governance and Risk Management Team Leader (NHS Tayside)
- Yvette Burgess: Director at Housing Support Enabling Unit
