Stage Two: Co-designing
The second stage of this project was undertaken over eight months from early May until December 2014.
During this eight-month phase the project lead, Fiona Munro, was supported by Stuart Muirhead, a project manager within Iriss's Evidence Informed Practice Team, to run a series of monthly co-design workshops within Tayside. Three Masters of Design for Services students from Duncan of Jordanstone College of Art & Design also provided additional support helping to run the workshops during this phase of the project.
These workshops were designed to support a range of health and social care practitioners working in Tayside to work alongside older people and informal carers who had recently experienced the local discharge pathway. The Design Council's Double Diamond Methodology was used to identify issues with the current discharge pathway and to co-design interventions for local implementation.
“Just go for it and get involved you will be amazed what you learn and you will find it most enjoyable.”
—Reflections from an Older Person involved in the Working Groups
“The experience has been so valuable to actually meet people face to face and listen and process information which can then be used to develop, validate or change what has been learned.”
—Reflections from a Practitioner involved in the Working Groups
More information about the specific activities used during these workshops can be found in this audio update from Stuart:
The Scottish Co-Production Network has also published a case study of the co-production approach applied during these workshops. This provides a helpful overview of the co-design methodology used and some of the learning gained by the group as a whole.
Key problems
“As we moved into the sessions looking at the pathways I quickly focused on language and the importance to make it clear and not full of jargon or buzz words but plain and simple for everyone to understand. Professional barriers were quickly removed as we were aware that we all wanted the same outcome, an outcome that was to provide an excellent pathway of Hospital to Home for the person involved.”
—Reflections from a Practitioner involved in the Working Groups
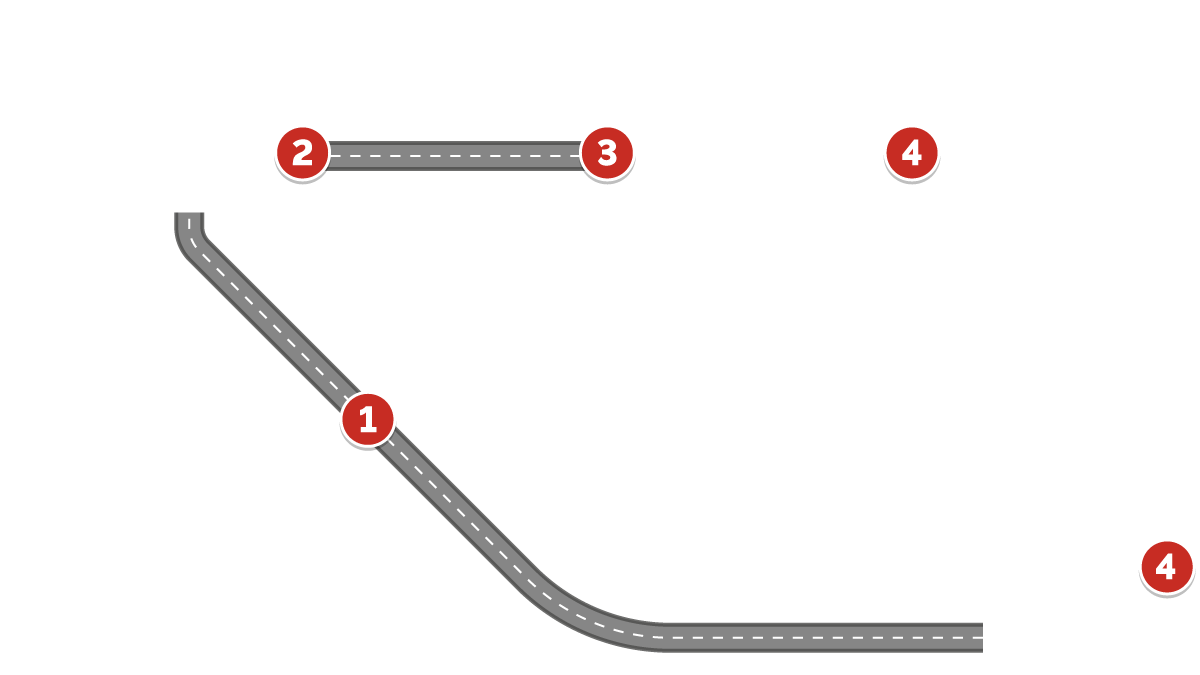
The group worked collaboratively to identify the key problems that prevent an older person from having a positive experience during their transition from hospital to home. This process identified problems at four key stages. Click on the map icons below for more…

Key learning
“Our outcomes quickly became apparent that it was a pathway for the person or people involved and we all wanted to get it right.”
—Reflections from a Practitioner involved in the Working Groups
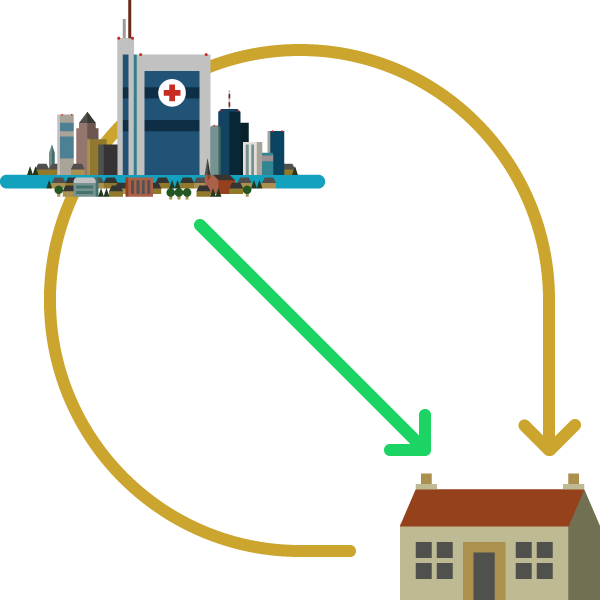
One of the key learning outcomes from this phase of the project was the varying perspectives of the pathway from hospital to home.
The pracitioners' view
Practitioners, as a group, illustrated the pathway as starting in the hospital and ending when the older person is discharged and returns home or to a homely setting.
The non-pracitioners' view
Non-practitioners in the group, on the other hand, illustrated that they see the pathway starting and finishing at home, with the hospital playing only a small part of their journey.
Shifting the perspective of practitioners to match that of the people within their care will ultimately help to lead to a more person-centred pathway that focuses on the person’s desired outcomes.
Pracitioners' view
Non-pracitioners' view
Identified solutions
“I believe it is important that problems with communication are addressed. I would like to see at least one of this group's recommendations going forward and to hear that it is actually working in practice.”
—Reflections from an Older Person involved in the Working Groups
1. An admission coordinator
There were concerns about the quality of the information gathered at the point of an unplanned admission to hospital and how this is then shared through the pathway within hospital and into the community.
The introduction of an admission coordinator may resolve some of these issues. This coordinator would be responsible for gathering and recording all necessary information at the point of the older person’s unplanned admission to hospital and ensuring that this information is passed on appropriately throughout the hospital staff. In addition, they would also take responsibility for notifying the key services already involved in the older person’s care in the community (GP, Social Services and third sector organisations) and involving them in the discharge planning process.
This process could be informed by the success of the planned admission planning already in place. In response to the problems identified, this approach would help to ensure that the older person:
- Has their needs considered from the start of their pathway
- Is kept at the centre of all discussions
- Has their information only passed on to those who need it
- Isn’t asked for the same information repeatedly
- Has a person they know they can turn to for further information and reassurance
In addition this would also help to ensure:
- Existing forms are utilised more effectively and appropriately
- Better communication between the hospital and community based staff from the point of admission, rather than discharge
- This in turn would prepare the community based teams for discharge at an earlier stage and help to prevent unnecessary delayed discharges
- All practitioners share the same good communication strategies
2. A named practitioner following the older person
Information is not always shared with the older person, their family or informal carers and they don’t always know what to expect, what is happening next or when their discharge is likely to be.
The number of practitioners involved in an older person’s hospital stay and discharge only compounds these issues.
The group proposed, therefore, that one practitioner take responsibility for all information shared with and about the older person. This person could also have the role of the admission and/or discharge coordinator, mentioned above.
In response to the problems identified previously, this approach would help to ensure that the older person:
- Always knows who to ask questions if they have any concerns or uncertainties
- Has their needs identified and addressed throughout their hospital stay and discharge
- Always has the information about their care with them - “nothing about me without me”
In addition this would also help to ensure:
- One practitioner has responsibility for the older person’s information and for ensuring it is shared appropriately within the hospital and community
- An effective communication link between the community and hospital based care
3. ‘Discharge’ at home
One of the recurring issues arising through this project was how older people feel when they are discharged and how this can contribute to them not experiencing a positive pathway from hospital to home.
Being discharged from hospital can often be as traumatic for an older person as when entering the hospital at the start of their journey through acute care. They often don’t know how they will cope at home, who will support them and what to expect generally about their changed capabilities. A hospital stay will often reduce an older person’s confidence, mobility and independence as well as increasing their frailty. All of this constitutes a number of unwanted emotions such as fear, anxiety and stress. These are furthered by a lack of communication about when they are likely to return home.
Lack of appropriate assessment of an older person’s home prior to discharge and delays in necessary housing adaptations only create additional problems once the older person returns home. This increases the likelihood that they will be readmitted.
Considering these concerns, recommendation was made that older people be discharged from the hospital service once they are in their home and they are happy to be so, rather than at the point when they leave acute care.
In response to the problems identified, this approach would help to ensure that the older person:
- Receives support once at home that is appropriate to their individual needs
- Remains in control of when they are discharged
- Has time to adapt to and understand that their circumstances and/or capabilities may have changed
- Has overnight support within the community through communication links to acute care
- Has control over decisions about their care – these are made with them in a setting in which they are comfortable (i.e. their own home)
- Is able to better manage the unexpected concerns that may arise
- Doesn’t feel socially isolated following discharge
- Is always involved in discussions and in control of what happens to them
In addition this would also help to ensure:
- An overlap between hospital and community based practitioners
- Integrated working
- Person-centred care
The people
This eight-month co-design phase of the project was greatly supported by a number of practitioners, older people and informal carers in Tayside. We have also been fortunate enough to gain support and insight from local University of Dundee Masters of Design for Services Graduates.
With special thanks for their time and input, and with their permission, some of those involved are listed below:
NHS Tayside
- Caroline McQuillian: Associate Nurse Director NHS Tayside, Nursing & Midwifery Directorate
- Cesar Rodriguez: Clinical Lead Older People in Acute Care Collaborative, NHS Tayside
National Project Advisory Group
- Bernie Campbell: Scottish Care
- David Strathearn: CCPS Associate / Voluntary Sector Advisor
- Diane McCulloch: Head of Community Care, Social Work Department, at Dundee City Council
- Miles Witham: Clinical Reader in Ageing and Health at NHS Tayside/University of Dundee School of Medicine
- Roy Soiza: Consultant Geriatrician & Honorary Clinical Senior Lecture at NHS Grampian
Tayside Project Working Group
- Andrea Blyth: Occupational Therapist, Community Rehabilitation Team, Dundee
- Amanda Clements: Nurse Coordinator Intermediate Care, Assessment Clinic for the Elderly Manager, Perth and Kinross CHP
- Arlene Ogilvie: Social Worker, Community Mental Health Team Older People, Dundee
- Catherine Davidson: Angus Discharge Co-ordinator within Social Work Department, Dundee
- Christina Cooper: Project Coordinator, Reshaping Care for Older People Change Fund, Dundee Voluntary Action
- Donna Laird: Team Leader District Nursing, Dundee
- Elizabeth Fairgrieve: Service User, Tayside
- Iain Paton: Project Officer, Special Needs Unit, Housing Investment Unit
- Ian Leitch: Informal Carer, Tayside
- Jean Cook: Service User, Tayside
- Karen Gall: Team Leader, Dundee Discharge Team
- Karen Lesslie: Acting Team Manager, Enablement & Support/CMHT, Dundee
- Kristy Whitton: Nurse Practitioner, Medicine for the Elderly Team, South Angus
- Margaret Hume: Informal Carer, Tayside
- Michael Carson: Locality Pharmacist, Dundee CHP
- Olivia Robertson: Head of Nursing, Medicine for the Elderly, NHS Tayside
- Stan Eggie: Service User, Tayside
- Tanya Gold: Social Worker, Social Work Department, Ninewells Hospital
- Tracey Passway: Clinical Governance and Risk Management Team Leader, NHS Tayside
- Willis Brown: Service User, Tayside
University of Dundee Masters of Design for Services Graduates
- Aishwarya Iyengar: Service Design Graduate, University of Dundee
- Lorri Smyth: Service Design Graduate, University of Dundee
- Yiqiu Wang: Service Design Graduate, University of Dundee
